Almost everyone has experienced heartburn. About 25 million American adults suffer daily from (esophageal reflux, sometimes referred to as gastroesophageal reflux disease (GERD) or heartburn). It is that burning sensation felt in the chest and sometimes in the neck. GERD is caused by acid, normally found in the stomach, refluxing or splashing up into the esophagus — the muscular tube that connects the throat to the stomach. Occasional esophageal reflux is usually nothing to be concerned about. However, anyone who has esophageal reflux on a regular basis should consult a physician. Constant exposure to stomach acid can irritate the lining of the esophagus and cause other medical problems.
What is GERD?
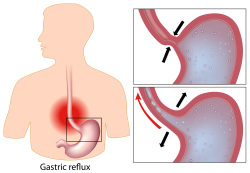
The esophagus carries food and liquid into the stomach. At the lower end of the esophagus where it enters the stomach, there is a muscular ring called the lower esophageal sphincter (LES). The LES should remain tightly closed, except to allow food and liquid to pass into the stomach. Esophageal reflux occurs when the LES is not functioning properly allowing stomach acid to flow freely up into the esophagus. It may relax for periods of time throughout the day and night, or it may be constantly too weak to function effectively. How severe the disease becomes depends on how weakened the LES is, and the amount and duration of acid refluxed into the esophagus.
It is also common to find a hiatal hernia complicating GERD. With a hiatal hernia, the upper part of the stomach actually pushes up into the chest cavity through an enlarged opening in the diaphragm. The diaphragm is the thin, flat muscle that separates the lungs from the abdomen. A hiatal hernia frequently decreases the LES’s ability to prevent regurgitation of stomach contents.
Symptoms and Causes of GERD
Frequent heartburn is the most common symptom. However, patients may also experience some of the following:
- Burning in chest
- Sour or bitter taste in mouth, especially during the night
- Hoarseness
- Trouble swallowing
- Repeatedly feeling a need to clear the throat
- Difficulty swallowing food or liquid
- Chronic cough
- Worsening of symptoms after eating, or when bending over or lying down
Certain diet and lifestyle choices can contribute to the condition. For example, certain foods increase acid production, and fatty foods increase the time food remains in the stomach. Chocolate, peppermint, coffee, alcoholic beverages, and especially nicotine in cigarette smoke weaken or relax the LES. Obesity and pregnancy place added pressure on the upper abdomen. During pregnancy, the LES weakens for unknown reasons.
Complications
Complications can occur when GERD is severe or long-standing. Constant irritation of the esophagus by stomach acid can lead to inflammation, ulcers, and bleeding. Anemia or low blood count may develop. Over time, scarring and narrowing of the esophagus can also develop, making it difficult to swallow foods and liquids. This narrowing is called an esophageal stricture. Some patients develop a condition called Barrett’s esophagus, where there is change in the cells lining the esophagus. Barrett’s esophagus may be a forerunner of esophageal cancer.
Diagnosis of GERD
The diagnosis can usually be suspected by the physician, simply by taking the medical history. Beyond that, the physician may order an x-ray examination of the esophagus and stomach. For this x-ray, the patient swallows a liquid containing barium. This makes it possible to see the reflux and a hiatal hernia on the x-ray. Endoscopy (EGD) is the most important test for patients with GERD. It is done with the patient under sedation. The physician examines the lining of the esophagus and stomach with an endoscope. The EGD is helpful in determining the severity of the disease, and if Barrett’s tissue is present. Certain conditions, such as narrowing or stricture in the esophagus, can usually be corrected during this procedure. During an endoscopy, the physician can also look for signs of esophageal damage and perform a biopsy if Barrett’s changes have occurred.
There are other tests that are helpful. A pressure recording of the esophagus is called esophageal manometry. It measures the pressure in the LES and any abnormal muscle contractions in the main part of the esophagus. Finally, a 24-hour recording of the acidity in the esophagus is often helpful.
What is the treatment?
Treatment is aimed at reducing reflux and damage to the lining of the esophagus. Initial treatment is with lifestyle changes. Patients with GERD should follow these recommendations:
- Avoid eating anything within three hours before bedtime.
- Stop smoking. Nicotine in the blood weakens the LES.
- Avoid fatty foods, chocolate, spearmint, peppermint, caffeine, citrus fruits and juices, tomato products, pepper seasoning, and alcohol — especially red wine.
- Decrease portions of food at mealtime and avoid tight clothing or bending over after eating.
- Review all medications with the physician. Certain drugs can weaken the LES, allowing acid irritation of the esophagus.
- Elevate the head of the bed or mattress 6 to 8 inches. This helps prevent acid reflux especially when sleeping. Extra pillows by themselves are not very helpful.
- Lose weight if overweight. This may relieve upward pressure on the stomach and LES.
Lifestyle changes are often all that is needed to correct mild forms of GERD. When symptoms are moderate to severe, the physician will prescribe medications. There are two broad classes of medications used to reduce stomach acid production. For milder cases of GERD, histamine blockers are used. These include Zantac, Pepcid, Tagamet and Axid. The second category of medications are proton pump inhibitors. They include Prilosec, Prevacid, Protonix, Nexium and Dexilant as well as others. Proton pump inhibitors are used for more frequent or troublesome reflux. Both categories are generally safe, are available in generic form over the counter. Sometimes two medications are used when GERD is severe.
Some patients with GERD may need surgery to strengthen the LES. This procedure is called fundoplication. Previously this surgery required a major operation, often through the chest. It was a difficult operation for the patient, with a long recovery. It is now usually done by laparoscopy. This is a minimally invasive surgery, performed with a small incision at the naval and a few other points in the upper abdomen. The patient usually returns home 1-2 days after surgery, with few problems. Surgery, generally, is not considered until all other measures have been tried.
Summary
GERD is a common problem that requires medical attention when symptoms and tissue damage become troublesome. Fortunately, there is a great deal that can now be done about GERD. Lifestyle changes, medications, and even surgery can treat and correct GERD. Working together with the physician, a good medical program can almost always be developed to successfully treat the patient with GERD.