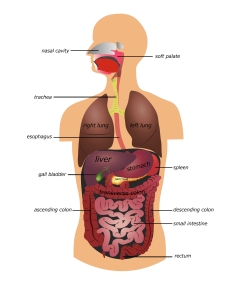
Heartburn is a burning sensation felt behind the breastbone and sometimes in the neck and throat. It is caused by stomach acid refluxing or splashing up into the esophagus — the muscular tube that connects the throat to the stomach. At the lower end of the esophagus where it enters the stomach, there is a strong muscular ring called the Lower Esophageal Sphincter (LES). The LES should remain tightly closed, except to allow food and liquid to pass into the stomach. Heartburn occurs when the LES opens at the wrong time.
Almost everyone has this occasionally, and it is nothing to be concerned about. However, heartburn that is severe or that occurs frequently over a long period of time can be harmful. This is known as Gastroesophageal Reflux Disease (GERD). If GERD is untreated, there is constant acid irritation to the lining of the esophagus, and complications can occur. About 1 in 10 patients with GERD are found to have a condition called Barrett’s esophagus. Those with Barrett’s esophagus are at slightly increased risk to develop cancer of the esophagus.
What is Barrett’s Esophagus?
The cells lining the esophagus differ from those lining the stomach or intestines, mainly because they have different functions. They also have a distinctly different appearance, so it is usually easy for a physician to tell them apart when examining the esophagus and stomach. Normally, there is an area at the end of the esophagus that marks the border between the cells of the esophagus and those of the stomach. Barrett’s esophagus is the abnormal growth of intestinal-type cells above this border, into the esophagus.
The Barrett’s cells may help protect the esophagus from acid exposure. It may protect the normal tissue in the esophagus against further damage by GERD. This may explain why the symptoms of GERD seem to lessen in some patients with Barrett’s esophagus.
Unfortunately, these tissue changes may be a forerunner of cancer of the lower esophagus, known as adenocarcinoma. Another type of cancer of the esophagus is squamous cell cancer. It is more often formed in the upper esophagus and is increased in those with a history of alcohol and tobacco abuse. Squamous cancers of the esophagus appear to be decreasing in the population, while the rate of adenocarcinoma is increasing sharply, especially in white males.
In time, the Barrett’s cells may develop abnormal changes known as dysplasia. Over a period of perhaps two to five years, the dysplasia may progress from low grade to high grade dysplasia, and finally to cancer. Fortunately, this happens only in about 1-5% of patients with Barrett’s esophagus.
We believe that the length of Barrett’s a person has impacts their risk so a person with five inches of Barrett’s is at higher risk than someone with one inch.
Cause and Symptoms
For unknown reasons, Barrett’s esophagus is found three times more often in males than in females. In some instances, Barrett’s esophagus appears to be congenital (present at birth). However, current evidence is strong that in most instances, it develops as a result of longstanding GERD.
Patients with Barrett’s usually have symptoms similar to those produced by chronic GERD, such as heartburn and reflux of stomach acid into the mouth. Some Barrett’s patients may also suffer from other complications of GERD, such as esophageal peptic ulcers and stricture — narrowing of the esophagus that comes from scarring. These facts are why it is important for patients with these symptoms to see their physicians regularly.
Diagnosis
Diagnosis of Barrett’s esophagus requires an examination called upper endoscopy or EGD (esophagogastroduodenoscopy). A barium x-ray is not accurate for detecting Barrett’s esophagus. An EGD is done with the patient under sedation. The physician examines the lining of the esophagus and stomach with a thin, lighted, flexible endoscope. Biopsies are performed, taking pieces of tissue to be examined under a microscope for abnormal cells and to assess their potential of becoming malignant. These changes include the term indefinite dysplasia where the pathologist may be uncertain of the changes. In this circumstance, medical treatment is intensified and repeat biopsies are performed in 6-12 months. Newer, gene testing can also be done on the biopsy to help assess the risk of progression towards cancer. When dysplasia is definite, some type of definite correction is often necessary.
Things Patients Can Do
Currently, there are no medications to reverse Barrett’s esophagus. However, it appears that treating the underlying GERD may slow the progress of the disease and prevent complications.
Following are some things the patient can do to help reduce acid reflux and strengthen the LES.
- Avoid eating anything within three hours before bedtime.
- Avoid smoking and tobacco products. Nicotine in the blood weakens the LES. Smoking increases the risk of cancer.
- Reduce consumption of fatty foods, milk, chocolate, mints, caffeine, carbonated drinks, citrus fruits and juices, tomato products, pepper seasoning, and alcohol.
- Eat smaller meals. Avoid tight clothing or bending over after eating.
- Review all medications with the physician. Certain drugs can actually weaken the LES.
- Elevate the head of the bed or mattress 6 to 8 inches. This helps to keep acid in the stomach. Pillows by themselves are not very helpful. Wedging pillows under the head tends to bend the body at the waist which can push more fluid back up into the esophagus.
- Lose weight if overweight. This may relieve upward pressure on the stomach and LES.
Medications
A certain category of drugs called proton pump inhibitors are the main tool used to reduce stomach acid. There are a number of these medications available. Some of the more common ones include Prilosec (omeprazole), Prevacid (lansoprazole), AcipHex (rabeprazole), Protonix (pantoprazole), Nexium (esomeprazole), and Dexilant (dexlansoprazole) taken once or twice a day. All of these are equally effective. Other acid reducing drugs such as Zantac, Pepcid, Axid, and Tagamet are also available. Reglan (metoclopramide) is a drug that can strengthen the LES and can help but carries potential side effects. A newer class of acid blocker medication include vonoprazan (Voquezna) and are a recent addition to the treatment options.
Surgery
Certain patients with GERD may need surgery to tighten the area around the LES. This type of surgery is called fundoplication. It is now done by laparoscopy. Laparoscopy is minimally invasive surgery, performed with small incisions at the naval and a few other points in the upper abdomen.
Treatments
A number of treatments have come available to eradicate the Barrett’s cells in those who develop dysplasia to suggest they may be at risk to develop cancer. It is important to remember that the vast majority of people with Barrett’s never develop dysplasia or cancer. In those patients who do develop dysplasia, however, we now have available a number of treatments to include cryotherapy and radio frequency ablation. Talk with your physician to decide what is best for you.
Monitoring
A diagnosis of Barrett’s esophagus requires regular monitoring by a physician. While it is thought that controlling GERD reduces the risk of developing cancer, this has not yet been definitely proven. Therefore, the physician must perform regular endoscopy exams and biopsies to look for dysplasia. Just how often these exams are repeated depends on how far the disease has advanced. If cancer is found, and depending on the stage, surgery to remove the esophagus may be necessary.
Treatment Options (for those with dysplasia or very early cancer)
There are numerous newer treatments constantly being studied. These involve the destruction or the targeted removal of the abnormal cells or nodules in the esophagus without the need for major surgery.
Summary
Barrett’s esophagus is a condition that may develop as a result of chronic GERD. Barrett’s tissue growing in the esophagus appears to be the body’s defense against continued stomach acid irritation. Yet, this tissue does not belong in the esophagus, and for a small number of patients, it increases the risk of developing cancer. While medications do not reverse Barrett’s, the likelihood of developing cancer and complications can probably be reduced with a combination of diet, lifestyle changes, medication, and/or surgery. A regular program of endoscopic examination and biopsy is essential to monitor the Barrett’s tissue. There are also a number of treatments available for those patients who develop dysplasia. By working closely with a physician, patients can expect good control of both GERD and Barrett’s, and an excellent long-term outcome.