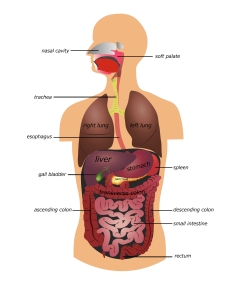
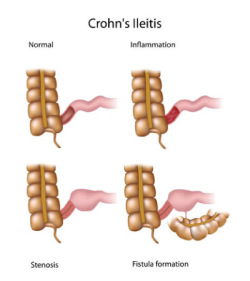
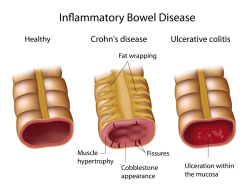
Crohn’s disease is a chronic, recurrent inflammatory disease of the intestinal tract. The intestinal tract has four major parts: the esophagus, or food tube; the stomach, where food is churned and digested; the long, small bowel, where nutrients, calories, and vitamins are absorbed; and the colon and rectum, where water is absorbed and stool is stored. The two primary sites for Crohn’s disease are the ileum, which is the last portion of the small bowel (ileitis, regional enteritis), and the colon (Crohn’s colitis). The condition begins as small, microscopic nests of inflammation which persist and smolder. The lining of the bowel can then become ulcerated and the bowel wall thickened. Eventually, the bowel may become narrowed or obstructed and surgery would be needed.
What Causes Crohn’s Disease?
There is now evidence of a genetic link as Crohn’s frequently shows up in a family group though we suspect that there are many genes that may contribute. In addition, there is evidence that the normal bacteria that grow in the lower gut may, in some manner, act to promote inflammation. The body’s immune system, which protects it against many different infections, is known to be a factor. There are still a number of unknowns about the cause of the disease. Fortunately, a great deal is known about the disease and especially its treatment.
Who Develops Crohn’s Disease?
The condition occurs in both sexes and among all age groups, although it most frequently begins in young people. Jewish people are at increased risk of developing Crohn’s, while African Americans are at decreased risk, which suggests a genetic component to this disease.
Symptoms
The symptoms of Crohn’s disease depend on where in the intestinal tract the disorder appears. When the ileum (ileitis) is involved, recurrent pain may be experienced in the right lower abdomen. At times, the pain mimics acute appendicitis. When the colon is the site, diarrhea (sometimes bloody) may occur, along with fever and weight loss. Crohn’s disease often affects the anal area where there may be a draining sinus tract called a fistula.
When the disease is active, fatigue and lethargy appear. In children and adolescents there may be difficulty gaining or maintaining weight.
Diagnosis
There is no one conclusive diagnostic test for Crohn’s disease. The patient’s medical history and physical exam are always helpful. Certain blood and stool tests are performed to arrive at a diagnosis. X-rays of the small intestine and colon may be ordered. In addition, a thorough exam of the entire colon (colonoscopy) is often the best way of diagnosing the problem when the disease is in the colon. Capsule endoscopy and MRI are also available to inspect the small intestine.
Course and Complications
The disorder often remains quiet and easily controlled for long periods of time. Most people with Crohn’s disease continue to pursue their goals in life, go to school, marry, have a family and work.
Some problems, outside the bowel, can occur. Arthritis, eye and skin problems, and — in rare instances — chronic liver conditions may develop. As noted, the disease can occur around the anal canal. Open sores called fissures can develop, which are often painful. A fistula can also form. This is a tiny channel that burrows from the rectum to the skin around the anus. In addition, when inflammation persists in the ileum or colon, narrowing and partial obstruction may occur. Surgery is usually required to treat this problem. When Crohn’s disease has been present for many years, there is an increased risk of cancer.
Treatment
Effective medical and surgical treatment is available for Crohn’s disease. It is particularly important to maintain good nutrition and health with a balanced diet, adequate exercise, and a positive, upbeat attitude. Six broad categories of medications are available to treat this disease:
- Cortisone or Steroids — These powerful drugs provide highly effective results. A large dose is often used initially to bring the disorder under quick control when the disease is severe. The drug is then tapered before it is discontinued, and other medications used to keep the disease under control. This medicine is administered by pill or enema. Prednisone is a common generic name.
- Anti-inflammation drugs — sulfasalazine (Azulfidine), Dipentum, Asacol, Delzicol, Rowasa, Lialda, Colazal, Apriso, Pentasa, and others belong to a group of drugs called the 5-aminosalicylates. These drugs are most useful in maintaining a remission, once the disease is brought under control. These are available in oral and enema preparations.
- Immune System Suppressors — These medications suppress the body’s immune system, which appears to be overly active and somehow aggravates the disease. The names of three of these commonly used medications are azathioprine (trade name: Imuran), 6 MP (trade name: Purinethol) and methotrexate. These drugs are particularly useful for long-term care. There are other potent immune-suppressing drugs that may be used in difficult cases.
- Biologics — These drugs belong to a group of medications that blocks the body’s inflammation response, called TNF, ICAM, anti-interleukins and others. Infliximab (Remicade), adalimumab (Humira) and certolizumab (Cimzia) are three such agents and are given either by injection or infusion. Vedolizumab (Entyvio) blocks the white cell’s ability to move outside the blood system. Ustekinumab (Stelera), risankizumab (Skyrizi) and mirikizumab (Omvoh) block certain proteins called interleukins that are generated as part of an inflammatory response. These are given as an injection. A final class of drugs are called Janus kinase (JAK) blockers. Upadacitinib (Rinvoq) and Tofacitinib (Xeljanz) block another set of inflammatory proteins call JAKs. As of this writing, these are not yet FDA approved for Crohn’s. These are taken orally. These blocking antibody drugs are proving to be very effective in many patients.
- Antibiotics — Since there is frequently a bacterial infection along with Crohn’s disease, antibiotics are used to treat this problem. Two that are commonly used are ciprofloxacin (trade name: Cipro) and metronidazole (trade name: Flagyl).
Diet and Emotions
There are no foods known to actually injure the bowel. However, during an acute phase of the disease, bulky foods, milk, and milk products may increase diarrhea and cramping. Generally, the patient is advised to eat a well-balanced diet, with adequate protein and calories. A multivitamin and iron supplement may be recommended by the physician if the disease is sufficiently active to impact absorption of essential minerals and vitamins. A diet rich in fruits and vegetables and low in processed foods is also encouraged. Finally, there is some research data to suggest foods that contain emulsifiers, commonly found in processed foods, can weaken the protective, mucus layer of the bowel wall. Examples include lecithin, tartaric acid, polyglycerol esters, sucrose esters. Read food labels. We feel it best to avoid these foods and maintain a diet focused on a largely plant based diet.
Stress, anxiety, and extreme emotions may aggravate symptoms of the disorder, but are not believed to cause it or make it worse. Any chronic disease can produce a serious emotional reaction, which can usually be handled through discussion with the physician.
Surgery
Surgery is commonly needed at some time during the course of Crohn’s disease. It may involve removing a portion of diseased bowel, or simply the draining of an abscess or fistula. In all cases, the guiding principle is to perform the least amount of surgery necessary to correct the problem. Surgery does not cure Crohn’s disease.
Summary
Most people with Crohn’s disease lead active lives with few restrictions. Although there is no known cure for the disorder, it can be managed with present treatments. For a few patients, the course of the disease can be more difficult and complicated, requiring extensive testing and therapy. Surgery sometimes is required. In all cases, follow-up care is essential to treat the disease and prevent or deal with complications that may arise.